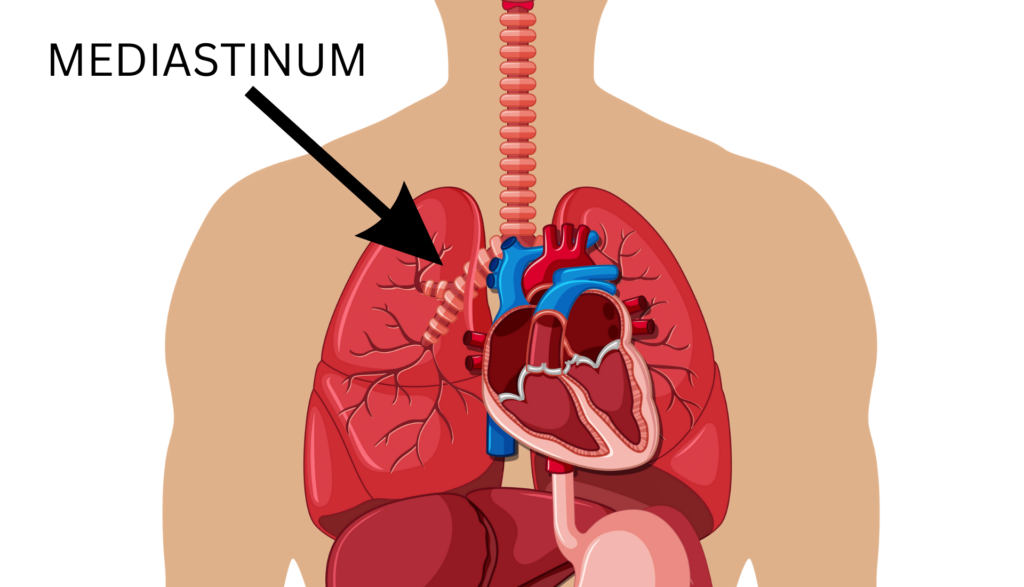
Mediastinum
Mediastinal Tumor – VATS and Open Surgery
Mediastinal tumors are essentially a (benign or malignant) growth in the space between the lungs and is the area between the breastbone and spinal column. Once the mediastinal tumor is diagnosed by biopsy, it’s treatment can range from a surgical removal to chemotherapy & Radiotherapy or to a combination of all the three modalities.
Video Assisted Thoracic Surgery (VATS), a minimally invasive procedure with or without Robotic assistance, is being progressively used for the treatment.. A tiny video camera is inserted to transmit the images of the inside of your chest. The surgeon carefully performs the surgery while the picture is being displayed on the monitor. The patients undergoing VATS experience, omparatively, less pain and rapid recovery over other treatments.Open surgery is needed
Myasthenia Gravis
The cause of myasthenia gravis is breakdown in the coordination between your muscles and nerves. It results in fatigue and weakening of muscles that are in your voluntary control.It may be associated with an enlargement of the Thymus gland or a thymic tumour called a thymoma
The treatment of myasthenia gravis involves controlling symptoms with medication and then removing the Thymus gland or thymoma because it has been shown to cause a remission in symptoms. Although myasthenia gravis can possibly affect people of any age, it is mostly seen in women below 40 and men above 60. The surgery is usually by VATS or Robotic Surgery.
Thymus Gland tumor
A tumour of the thymus gland is known as Thymoma. Thymus is a gland present in the anterior mediastinum that significantly helps in development of immune cells during childhood.
Quite surprisingly, the cause of thymus gland tumor is still unknown. Upto fifty percent of thymoma patients are asymptomatic. They are usually big if they cause symptoms due to pressure on the adjacent body organs including chest wall.Most often they are detected by an Xray done for some unrelated reason.
Primarily, surgery is the treatment for thymoma. Large tumours may need to be treated with chem or radiotherapy before surgery can be attempted. Its success, however, depends on the size and location of the tumor. If the surgical treatment remains unsuccessful, chemotherapy, radiation therapy or targeted therapy drugs can be resorted to.Your treatment should be planned by an experienced team for maximal success and we have the experience and the expertise.
Thymus Gland Carcinoma
Thymic Carcinoma, also known as Type C thymoma, is a more life threatening disease with a poorer long term outcome.
Just like Thymoma, generally, people affected by Thymic Carcinoma are asymptomatic. It is often found when imaging is done for an unrelated medical condition. However, some of the common symptoms are difficulty in breathing, chest pain, persistent cough, trouble in swallowing, depending on the organ which is being compressed by the tumour.
The commonly conducted for diagnosing thymus cancer are-
- Chest X-ray.
- Imaging Tests- PET, CT, MRI Scan.
- Biopsy.
The treatments available for thymus carcinoma may vary with the intensity/stage of the disease. Following treatments are used to cure thymus cancer-
The surest way to cure Thymic Carcinoma is surgery. It is used to remove the tumor and other tissue which the tumour has invaded. Radiation therapy, involving high energy X-rays, is used to kill cancer cells by destroying their DNA.
Chemotherapy kills the cancer cells using drugs.
Hormone therapy is useful when hormone receptors are found in the cancer cells.
Posterior Mediastinal Tumours and Masses
Nearly all tumors that occur in the posterior mediastinum are benign and are of nerve tissue origin. These tumors are thus ideally suited to minimally invasive, video-assisted thoracoscopic surgical (VATS) approaches. This approach can be used to resect all but the largest neurogenic tumors, bronchogenic cysts, and foregut duplication cysts. VATS permits far less discomfort and faster recovery than the traditional approach via thoracotomy, which requires a larger skin incision, more cutting of muscle, and spreading the ribs.Surgical expertise and experience is essential for good outcomes.
Mediastinal cysts
Mediastinal Cysts are mass-like structures that are encapsulated, contain fluid and lined with epithelium. Most of the mediastinal cysts are congenital. These include bronchogenic cysts, pericardial cysts, thymic cysts, foregut duplication cysts, pancreatic pseudocysts and esophageal duplication cysts.
The treatment for a mediastinal cyst or tumor, by and large, depends on the lesion which is being investigated. Most of the mediastinal cysts need surgical resection, especially large symptomatic bronchogenic cysts.
The treatment for a mediastinal cyst or tumor, by and large, depends on the lesion which is being investigated. Most of the mediastinal cysts need surgical resection, especially large symptomatic bronchogenic cysts.
Bronchogenic cysts are the most common type of mediastinal cysts. These are usually asymptomatic and found incidentally in the radioimaging of the chest. Larger bronchogenic cysts may result in obstruction and air entrapment in the respiratory airways.
In a radiograph, these cysts are usually fluid filled structures, with an occasional communication being developed leading to infection.
Some of the complications may include-
- Cyst Wall Ulceration.
- Formation of fistula or connection with the the Airways.
- Secondary Infection.
- Hemorrhage.
- Development of malignancy in the cysts such as- rhabdomyosarcoma, leiomyosarcoma, etc.
Ectopic Parathyroid Adenomas
In normal cases, the parathyroid glands exist in the neck around the thyroid gland.
Sometimes during migration in the embryo stage, these glands may move too far and end up being in the chest cavity. This is known as an Ectopic Parathyroid Gland. These glands can hyperfunction and can cause a bone destroying disease called hyperparathyroidism. This needs specialised surgery.
This type of surgery needs to be performed by a highly specialized surgeon as it has chances to be unsuccessful in the first attempt. We have the experiencea nd expertise to handle this rare condition by minimally invasive surgery.
